Measure Description
The Total Per Capita Costs (TPCC) measure is a payment-standardized, annualized, risk-adjusted, and specialty-adjusted measure that evaluates the overall cost of care provided to beneficiaries attributed to clinicians, as identified by a unique Taxpayer Identification Number/National Provider Identifier (TIN-NPI). The Total Per Capita Costs measure can be reported at the TIN or the TIN-NPI level.
Stay up to date with the latest news regarding MACRA and MIPS.
Rationale
To support the efforts of providers who are working to provide high-quality care to their Medicare Fee-for-Service (FFS) beneficiaries, the TPCC measure provides meaningful information about the costs associated with delivering care to beneficiaries attributed to their TIN-NPIs.
The TPCC measure was originally developed for use in the Physician Value-Based Modifier program, and was updated (see Section 4.0 for details) for inclusion in the Merit-based Incentive Payment System (MIPS) cost performance category.
Overview of Measure Calculation
Using Medicare Part A and Part B claims, with certain exclusions, the TPCC measure calculates the risk-adjusted per capita costs for beneficiaries attributed to a clinician (TIN-NPI), with reporting at the TIN or the TIN-NPI level.
Measure Numerator:
The numerator for the measure is the sum of the annualized, risk-adjusted, specialty-adjusted Medicare Part A and Part B costs across all beneficiaries attributed to a TIN-NPI, within a TIN or TIN-NPI (depending on the level of reporting).
Measure Denominator:
The denominator for the measure is the number of all Medicare beneficiaries who received Medicare-covered services and are attributed to a TIN-NPI, within a TIN or TIN-NPI (depending on the level of reporting), during the performance period.
Eligibility and Exclusion Criteria:
Beneficiaries are excluded from the population measured if they meet any of the following conditions:
- were not enrolled in both Medicare Part A and Part B for every month during the performance period, unless part year enrollment was the result of new enrollment or death
- were enrolled in a private Medicare health plan (for example, a Medicare Advantage HMO/PPO or a Medicare private FFS plan) for any month during the performance period
- resided outside the United States, its territories, and its possessions during any month of the performance period
After applying the exclusions outlined above, all Medicare beneficiaries who received Medicare-covered services and are attributed to a TIN-NPI during the performance period are included in the calculation of the TPCC measure. Beneficiary attribution follows a two-step process (described in Section 3.0, Step 1) that assigns a beneficiary to a single TIN-NPI based on the amount of primary care services received and the clinician specialties that performed these services.
Data Source:
This measure is calculated from Medicare Part A and Part B final action claims for services provided during the performance period that include: inpatient hospital; outpatient hospital; skilled nursing facility; home health; hospice; durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS); and Medicare Part B Carrier (non-institutional physician/supplier) claims.
The measure also uses Medicare beneficiary enrollment data to capture patient characteristics. This measure does not require any additional measure submission by TIN-NPIs or TINs. Medicare Part A and Part B final action claims are used to attribute beneficiaries to TIN-NPIs for this measure, as described below.
Part D-covered prescription drug costs are not included in the calculation of the TPCC measure.
Detailed Measure Calculation Methodology
Calculation of the TPCC measure is divided into seven steps:
- Attribute beneficiaries to TIN-NPI,
- Calculate payment-standardized per capita costs,
- Annualize costs,
- Risk-adjust costs,
- Specialty-adjust costs,
- Calculate the TPCC measure for the TIN-NPI or TIN, and
- Report the TPCC measure for the TIN-NPI or TIN.
The following sections explain those steps in more detail.
Step 1: Attribute Beneficiaries to TIN-NPI
For the TPCC measure, beneficiaries are attributed to a single TIN-NPI in a two-step process that takes into account the level of primary care services received (as measured by Medicare allowed charges during the performance period) and the clinician specialties that performed these services. Only beneficiaries who received a primary care service during the performance period are considered in attribution.
The following two steps are used to attribute beneficiaries to a TIN-NPI for the TPCC measure:
a) A beneficiary is attributed to a TIN-NPI in the first step if the beneficiary received more primary care services (PCS) from primary care physicians (PCPs), nurse practitioners (NPs), physician assistants (PAs), and clinical nurse specialists (CNSs)3 in that TIN-NPI than in any other TIN-NPI or CMS Certification Number (CCN). If the beneficiary received more PCS from PCPs, NPs, PAs and CNSs from a CCN than any other TIN-NPI, this beneficiary would be attributed to the CCN, would not be attributed to any TIN-NPIs, and would be excluded from risk adjustment. Primary care services include evaluation and management services provided in office and other non-inpatient and non–emergency-room settings, as well as initial Medicare visits and annual wellness visits.4 If two TIN-NPIs tie for the largest share of a beneficiary’s primary care services, the beneficiary will be attributed to the TIN-NPI that provided primary care services most recently.
b) If a beneficiary did not receive a primary care service from any PCP, NP, PA, or CNS during the performance period, the beneficiary is attributed to a TIN-NPI in the second step if the beneficiary received more primary care services from non-primary care physicians within the TIN-NPI than in any other TIN-NPI or CCN. 5 If two TIN-NPIs tie for the largest share of a beneficiary’s primary care services, the beneficiary will be attributed to the non-primary care TIN-NPI that provided primary care services most recently. If the beneficiary received more
PCS from non-primary care physicians from a CCN than any TIN-NPI, this beneficiary would be attributed to the CCN, would not be attributed to any TIN-NPIs, and would be excluded
from risk adjustment. If the beneficiary did not receive any primary care service via PCP, NP, PA, CNS or non-primary care physician, then the beneficiary would not be attributed.
Step 2: Calculate Payment Standardized Per Capita Costs
The TPCC measure is payment standardized to take into account payment factors that are unrelated to the care provided (such as payments supporting larger Medicare program goals like indirect medical education add-on payments, or geographic variation in Medicare payment policies). This allows for a more equitable comparison across providers. More information on the payment standardization algorithm is available in an overview document titled “CMS Price (Payment) Standardization -Basics” and a more detailed document titled “CMS Price (Payment) Standardization -Detailed Methods,” at the webpage referenced in Section 4.0.
Step 3: Annualize Costs
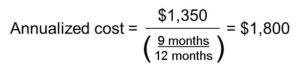
In performance year 2019, part year beneficiaries (those who were enrolled in Medicare Part A and Part B for only part of the year) may be attributed to TIN-NPIs if the reason for their part year enrollment was either that they were new enrollees in Medicare at some time other than the start of the calendar year or they died during the calendar year. In order to ensure valid comparisons between TIN-NPIs with part year beneficiaries and those without any part year beneficiaries, CMS annualizes the costs of part year beneficiaries before calculating the TPCC measure by dividing the total payment standardized costs for each beneficiary for the calendar year by the fraction of the year the beneficiary had both Medicare Part A and Part B coverage. For example, if a beneficiary had both Medicare Part A and Part B coverage from January through September, died in October, and had total costs of $1,350 over 9 months of full coverage, then the beneficiary’s annualized costs would be equal to $1,800:
For the purpose of this explanatory document, all subsequent instances of “cost” refer to “annualized, payment-standardized cost.”
Step 4: Risk-Adjust Costs
Risk adjustment accounts for beneficiary-level risk factors that can affect medical costs, regardless of the care provided. To estimate the expected per capita cost for each beneficiary, the TPCC methodology uses an ordinary least squares regression model to risk adjust for two measures of beneficiary risk. Prior to estimation of the regression model, extreme values of per capita costs are adjusted in a process called Winsorization: the top and bottom 1 percentile of the distribution of beneficiary costs is replaced with the 99th and 1st percentile value.
The two measures of beneficiary risk used in the risk adjustment algorithm are the beneficiary’s CMS-Hierarchical Condition Category (CMS-HCC) risk score and End Stage Renal Disease (ESRD) status. To ensure that the model measures the influence of health status (as measured by diagnoses) on the treatment provided (costs incurred), rather than capturing the influence of treatment on a beneficiary’s health status, the risk adjustment model uses prior year (2018) risk factors to predict current year (2019) total per capita costs. The CMS-HCC model generates a risk score for each beneficiary that summarizes each beneficiary’s expected cost of care relative to other beneficiaries. Separate CMS-HCC models exist for new enrollees and continuing enrollees. The new enrollee model accounts for each beneficiary’s age, sex, disability status, original reason for Medicare entitlement (age or disability), and Medicaid eligibility, and is used when a beneficiary has less than 12 months of medical history. The community model is used when a beneficiary has at least 12 months of medical history. The community model includes the same demographic information as the new enrollee model but it also accounts for clinical conditions as measured by Hierarchical Condition Categories (HCCs). A CMS-HCC risk score of 1 indicates risk associated with expenditures for the average beneficiary nationwide. A beneficiary risk score greater than 1 indicates above average risk and a risk score less than 1 indicates below average risk.
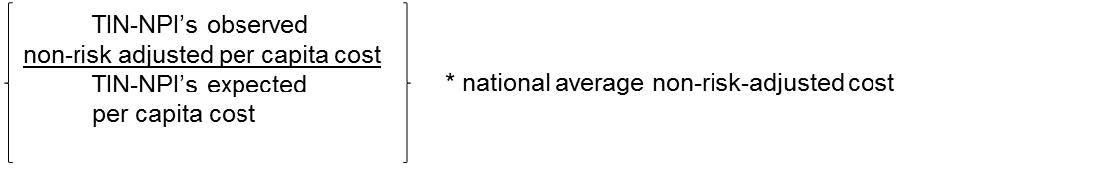
Risk-adjusted total per capita costs are then calculated to compare the TIN’s or TIN-NPI’s actual per capita costs with its expected per capita costs. A TIN’s or TIN-NPI’s risk-adjusted costs are calculated as the ratio of the TIN’s or TIN-NPI’s observed non–risk-adjusted total per capita costs to its expected total per capita costs, multiplied by the average non–risk-adjusted costs across all beneficiaries who are attributed to any TIN-NPI nationwide. The observed total per capita costs and expected total per capita costs in the ratio are both averaged across all beneficiaries attributed to TIN-NPIs in the TIN (or across all beneficiaries attributed to the TINNPI, in the case of TIN-NPI reporting). For example, the below figure shows how a TIN-NPI’s risk-adjusted total per capita cost would be calculated (the example shows “TIN-NPI calculation,” but “TIN calculation” would be done the same way):
TIN-NPI’s risk-adjusted per capita cost =
To summarize, the risk-adjusted total per capita cost is calculated using the following steps:
a)Replace the top and bottom 1 percentile of the distribution of beneficiary costs with the 99th and 1st percentile value, respectively (referred to as Winsorization).
b)Determine the expected total per capita cost based on risk adjustment algorithms that account for the beneficiary risk score – based on age, sex, disability status, original reason for entitlement (age or disability), Medicaid eligibility, and CMS-HCCs (for continuing enrollees only) – and ESRD status of attributed beneficiaries.
c)Compute the ratio of the TIN’s or TIN-NPI’s observed total per capita cost to its expected total per capita cost.
d)Multiply the TIN’s or TIN-NPI’s observed-to-expected ratio by the average non–risk-adjusted cost across all beneficiaries attributed to any TINs or TIN-NPIs. The result is the TIN’s or TINNPI’s risk-adjusted total per capita cost.
Step 5: Specialty-Adjust Costs
CMS recognizes that costs vary across specialties and across TINs or TIN-NPIs with varying specialty mixes. To support the goal of comparing TINs’ or TIN-NPIs’ costs more accurately to an expected cost that is reflective of their practice, CMS applies specialty adjustment to the TPCC measure. Specialty adjustment is different from risk adjustment. Specialty-adjusted costs for a TIN with a disproportionate number of eligible professionals in specialties with high national average costs, or for a TIN-NPI with those specialties, will be lower than the TIN’s or TIN-NPI’s non–specialty-adjusted costs, because the expected costs will exceed the average cost across all TINs or TIN-NPIs; similarly, specialty-adjusted costs will be higher than non– specialty-adjusted costs for TINs that have a disproportionate number of clinicians in specialties with low national average costs, or for TIN-NPIs with those specialties.
Eligible professional specialties are identified based on the CMS specialty code listed with the most allowable charges on Medicare Part B claims for services rendered by the professional during the performance year. In the case of a tie, the specialty listed on the most recent claim is selected.
Once a single specialty is identified for each TIN-NPI, the specialty is determined (whether or not it is an eligible professional) based on the CMS specialty code table. Then, only eligible professionals are included, and CMS adjusts the cost measures to account for each TIN-NPI’s specialty and each TIN’s specialty composition using three steps:
Step 5.1: Calculate a national average per capita cost for each specialty
First, calculate a national average per capita cost for each specialty. This national specialty-specific cost is the weighted average of each TIN’s or TIN-NPI’s risk-adjusted costs. The weights reflect the number of beneficiaries attributed to each TIN or TIN-NPI, as well as the number and share of practitioners of the relevant specialty in each TIN or TIN-NPI. For TIN-NPIs, there will be only one eligible professional, so the share will be one, or not weighted.
Step 5.2: Estimate the specialty-adjusted expected cost
Second, estimate the specialty-adjusted expected cost. Specialty-adjusted expected cost for the TIN is calculated by weighting the national specialty-specific cost by the Part B line provider payment share within the TIN. Specialty-adjusted expected cost for a TIN-NPI is the national specialty-specific cost for the specialty of that TIN-NPI, and since we only have 1 specialty for a TIN-NPI, the national expected cost for that specialty, calculated in step 5.1, is used.
Step 5.3: Construct the specialty-adjusted cost
Last, construct the ratio of risk-adjusted cost to specialty-adjusted expected cost. Multiply this ratio by the national average total per capita cost of all TINs or TIN-NPIs regardless of size.
Step 6: Calculate TPCC Measure
Measure calculation for TIN or TIN-NPI is completed in Step 5.3 above. The measure constructed in Steps 1-5 can be equivalently expressed in the manner implied by the numerator and denominator in Section 2.0: The sum of risk-adjusted, specialty-adjusted total per capita cost across all attributed beneficiaries for a TIN or TIN-NPI (depending on the level of reporting), divided by the number of attributed beneficiaries for the TIN or TIN-NPI.
Step 7: Report TPCC Measure for Each TIN-NPI or TIN
Although TPCC is attributed at the TIN-NPI level, reporting can be at either the TIN or TIN-NPI level. Under MIPS, the case minimum for reporting is 20 episodes, regardless of reporting level.
Additional References
For more information about the methodology used in payment standardization, please refer to the CMS Price (Payment) Standardization documents on QualityNet.
More details on MIPS may be found in the CY 2019 (83 FR 59767 – 59856) Physician Fee Schedule Final Rule, including updates from previous versions of TPCC.
Tables
The following tables present variables used to calculate the TPCC measure, as referenced in Section 3.0.
Table 1. HCCs included in the CMS-HCC risk adjustment model
| Indicator Variable | Description Label |
|---|---|
| HCC1 | HIV/AIDS |
| HCC2 | Septicemia, Sepsis, Systemic Inflammatory Response Syndrome/Shock |
| HCC6 | Opportunistic Infections |
| HCC8 | Metastatic Cancer and Acute Leukemia |
| HCC9 | Lung and Other Severe Cancers |
| HCC10 | Lymphoma and Other Cancers |
| HCC11 | Colorectal, Bladder, and Other Cancers |
| HCC12 | Breast, Prostate, and Other Cancers and Tumors |
| HCC17 | Diabetes with Acute Complications |
| HCC18 | Diabetes with Chronic Complications |
| HCC19 | Diabetes without Complication |
| HCC21 | Protein-Calorie Malnutrition |
| HCC22 | Morbid Obesity |
| HCC23 | Other Significant Endocrine and Metabolic Disorders |
| HCC27 | End-Stage Liver Disease |
| HCC28 | Cirrhosis of Liver |
| HCC29 | Chronic Hepatitis |
| HCC33 | Intestinal Obstruction/Perforation |
| HCC34 | Chronic Pancreatitis |
| HCC35 | Inflammatory Bowel Disease |
| HCC39 | Bone/Joint/Muscle Infections/Necrosis |
| HCC40 | Rheumatoid Arthritis and Inflammatory Connective Tissue Disease |
| HCC46 | Severe Hematological Disorders |
| HCC47 | Disorders of Immunity |
| HCC48 | Coagulation Defects and Other Specified Hematological Disorders |
| HCC54 | Drug/Alcohol Psychosis |
| HCC55 | Drug/Alcohol Dependence |
| HCC57 | Schizophrenia |
| HCC58 | Major Depressive, Bipolar, and Paranoid Disorders |
| HCC70 | Quadriplegia |
| HCC71 | Paraplegia |
| HCC72 | Spinal Cord Disorders/Injuries |
| HCC73 | Amyotrophic Lateral Sclerosis and Other Motor Neuron Disease |
| HCC74 | Cerebral Palsy |
| HCC75 | Myasthenia Gravis/Myoneural Disorders, Inflammatory and Toxic Neuropathy |
| HCC76 | Muscular Dystrophy |
| HCC77 | Multiple Sclerosis |
| HCC78 | Parkinson’s Disease and Huntington’s Disease |
| HCC79 | Seizure Disorders and Convulsions |
| HCC80 | Coma, Brain Compression/Anoxic Damage |
| HCC82 | Respirator Dependence/Tracheostomy Status |
| HCC83 | Respiratory Arrest |
| HCC84 | Cardio-Respiratory Failure and Shock |
| HCC85 | Congestive Heart Failure |
| HCC86 | Acute Myocardial Infarction |
| HCC87 | Unstable Angina and Other Acute Ischemic Heart Disease |
| HCC88 | Angina Pectoris |
| HCC96 | Specified Heart Arrhythmias |
| HCC99 | Cerebral Hemorrhage |
| HCC100 | Ischemic or Unspecified Stroke |
| HCC103 | Hemiplegia/Hemiparesis |
| HCC104 | Monoplegia, Other Paralytic Syndromes |
| HCC106 | Atherosclerosis of the Extremities with Ulceration or Gangrene |
| HCC107 | Vascular Disease with Complications |
| HCC108 | Vascular Disease |
| HCC110 | Cystic Fibrosis |
| HCC111 | Chronic Obstructive Pulmonary Disease |
| HCC112 | Fibrosis of Lung and Other Chronic Lung Disorders |
| HCC114 | Aspiration and Specified Bacterial Pneumonias |
| HCC115 | Pneumococcal Pneumonia, Empyema, Lung Abscess |
| HCC122 | Proliferative Diabetic Retinopathy and Vitreous Hemorrhage |
| HCC124 | Exudative Macular Degeneration |
| HCC134 | Dialysis Status |
| HCC135 | Acute Renal Failure |
| HCC136 | Chronic Kidney Disease, Stage 5 |
| HCC137 | Chronic Kidney Disease, Severe (Stage 4) |
| HCC157 | Pressure Ulcer of Skin with Necrosis Through to Muscle, Tendon, or Bone |
| HCC158 | Pressure Ulcer of Skin with Full Thickness Skin Loss |
| HCC161 | Chronic Ulcer of Skin, Except Pressure |
| HCC162 | Severe Skin Burn or Condition |
| HCC166 | Severe Head Injury |
| HCC167 | Major Head Injury |
| HCC169 | Vertebral Fractures without Spinal Cord Injury |
| HCC170 | Hip Fracture/Dislocation |
| HCC173 | Traumatic Amputations and Complications |
| HCC176 | Complications of Specified Implanted Device or Graft |
| HCC186 | Major Organ Transplant or Replacement Status |
| HCC188 | Artificial Openings for Feeding or Elimination |
| HCC189 | Amputation Status, Lower Limb/Amputation Complications |
Table 2. Healthcare Common Procedure Coding System (HCPCS) Primary Care Service Codes
| HCPCS Codes | Brief description |
|---|---|
| 99201–99205 | New patient, office, or other outpatient visit |
| 99211–99215 | Established patient, office, or other outpatient visit |
| 99304–99306 | New patient, nursing facility care |
| 99307–99310 | Established patient, nursing facility care |
| 99315–99316 | Established patient, discharge day management service |
| 99318 | New or established patient, other nursing facility service |
| 99324–99328 | New patient, domiciliary or rest home visit |
| 99334–99337 | Established patient, domiciliary or rest home visit |
| 99339–99340 | Established patient, physician supervision of patient (patient not present) in home, domiciliary, or rest home |
| 99341–99345 | New patient, home visit |
| 99347–99350 | Established patient, home visit |
| 99487, 99489 | Complex chronic care management |
| 99495-99496 | Transitional care management |
| 99490 | Chronic care management |
| G0402 | Initial Medicare visit |
| G0438 | Annual wellness visit, initial |
| G0439 | Annual wellness visit, subsequent |
| G0463 | Hospital outpatient clinic visit (Electing Teaching Amendment hospitals only) |
Table 3. CMS Specialty Codes for PCPs and Non-Physician Practitioners Included in the First Step of Attribution
| Specialty Description (CMS Specialty Code) |
|---|
| Primary Care Physicians |
| General Practice (01) |
| Family Practice (08) |
| Internal Medicine (11) |
| Geriatric Medicine (38) |
| Non-physician Practitioners |
| Clinical Nurse Specialist (89) |
| Nurse Practitioner (50) |
| Physician Assistant (97) |
Table 4. Medical Specialists, Surgeons, and Other Physicians Included in the Second Step of Attribution
| Specialty Description (CMS Specialty Code) | |
|---|---|
| Medical Specialists | Other Physicians |
| Addiction Medicine (79) | Anesthesiology (05) |
| Allergy/Immunology (03) | Chiropractic (35) |
| Cardiac Electrophysiology (21) | Diagnostic Radiology (30) |
| Cardiology (06) | Emergency Medicine (93) |
| Critical Care (Intensivists) (81) | Interventional Radiology (94) |
| Dermatology (07) | Nuclear Medicine (36) |
| Dentist (C5) | Optometry (41) |
| Endocrinology (46) | Pain Management (72) |
| Gastroenterology (10) | Pathology (22) |
| Geriatric Psychiatry (27) | Pediatric Medicine (37) |
| Hematology (82) | Podiatry (48) |
| Hematology/Oncology (83) | Radiation Oncology (92) |
| Hospice and Palliative Care (17) | Single or Multispecialty Clinic or Group Practice (70) |
| Infectious Disease (44) | Sports Medicine (23) |
| Interventional Cardiology (C3) | Unknown Physician Specialty (99) |
| Interventional Pain Management (09) | |
| Medical Oncology (90) | |
| Nephrology (39) | |
| Neurology (13) | |
| Neuropsychiatry (86) | |
| Osteopathic Manipulative Medicine (12) | |
| Physical Medicine and Rehabilitation (25) | |
| Preventive Medicine (84) | |
| Psychiatry (26) | |
| Pulmonary Disease (29) | |
| Rheumatology (66) | |
| Sleep Medicine (C0) | |
| Surgeons | |
| Cardiac Surgery (78) | |
| Colorectal Surgery (28) | |
| General Surgery (02) | |
| Gynecological/Oncology (98) | |
| Hand Surgery (40) | |
| Maxillofacial Surgery (85) | |
| Neurosurgery (14) | |
| Obstetrics/Gynecology (16) | |
| Ophthalmology (18) | |
| Oral Surgery (Dentists Only) (19) | |
| Orthopedic Surgery (20) | |
| Otolaryngology (04) | |
| Peripheral Vascular Disease (76) | |
| Plastic and Reconstructive Surgery (24) | |
| Surgical Oncology (91) | |
| Thoracic Surgery (33) | |
| Urology (34) | |
| Vascular Surgery (77) | |
Table 5. Practitioners and Therapists not included in the First or Second Step of Attribution
| Specialty Description (CMS Specialty Code) |
|---|
| Practitioners |
| Anesthesiologist Assistant (32) |
| Audiologist (Billing Independently) (64) |
| Certified Nurse Midwife (42) |
| Certified Registered Nurse Anesthetist (43) |
| Clinical Psychologist (68) |
| Clinical Psychologist (Billing Independently) (62) |
| Licensed Clinical Social Worker (80) |
| Registered Dietician/Nutrition Professional (71) |
| Therapists |
| Occupational Therapist in Private Practice (67) |
| Physical Therapist in Private Practice (65) |
| Speech Language Pathologists (15) |
